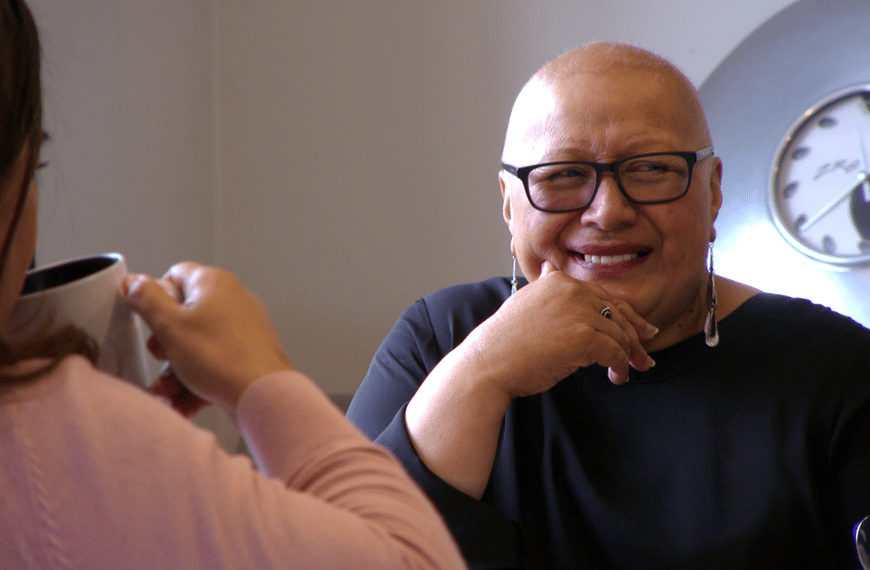
A new mental health agency will allow Pasifika patients in south Auckland to be seen by a professional the day they seek help.
Pasifika Medical Association (PMA) chief executive Debbie Sorensen says far too many people only get the help they need when they’ve reached their breaking point and in some cases ended up in police custody.
The Pacific Mental Health Commissioner was officially launched last week, aiming to ensure people are seen before they become really sick.
The agency will be funded by PMA and Te Whatu Ora. The services will be delivered through the Pasifika Futures’ Ngalu Fānifo mental health service.
Sorensen said it is keen to improve access in areas like south Auckland.
“Mental health in a Pacific context is not being catered for by mainstream mental health services and we see a high need for this to be addressed,” she said.
Sorensen said the services will operate alongside existing primary health and community services at eight different sites in Auckland, including at the Fono in Manurewa, Fonua Ola in Ōtāhuhu and Etu Pasifika South Auckland, in Manukau.
She said there has been an increase in depression and anxiety based conditions in the Pasifika community in recent years, despite the fact the numbers of people with more severe mental illnesses like schizophrenia and bipolar disorder have remained the same.
“But if you intervene early at a primary care level you can prevent these people ending up in hospital,” Sorensen said.
Mental Health Foundation chief executive Shaun Robinson said the new agency was one of a number seeking to provide early intervention services.
“The bottom line is it’s a good idea and is one of the advances we’re now seeing in mental health services,” Robinson said.
“It’s a significant step in the right direction. And making sure there are different services for different populations is really important.”
In the 2019 Budget, the Government committed $455 million towards expanding “access and choice” for services for people with mild to moderate mental health and addiction distress.
A Te Whatu Ora (Counties Manukau) report this month said Māori and Pacific people with mental health conditions were more likely to miss out on early interventions that might prevent their “progression to more significant ill-health”.
It said patients and their families were “at times reluctant to engage with clinical providers even if face-to-face and virtual services continued to be offered, and this created additional challenges for engagement post discharge”.
The report said in 2021/22 an average of 89% of patients discharged from Counties Manukau Health’s Tiaho Mai acute inpatient mental health unit were back in contact within seven days of discharge.