Public Interest Journalism funded through NZ On Air
By Kim Meredith of Local Democracy Reporting
Pacific peoples fertility in Aotearoa New Zealand will come under the microscope after a $1.2M study was awarded last month to a pair of young Tongan researchers.
Dr Edmond Fehoko from Otago University and Dr Zaramasina Clark from Te Herenga Waka, Victoria University were excited about being the recipients of such a substantial grant from the Health Research Council
They were still in shock when PMN spoke with them but both were hopeful the research would address what was now a major issue for Pacific communities and dispel the stereotype of Pacific people as prolific breeders.
In the early twenty noughts, cultural commentators speculated that Pacific communities’ tendency to have large families would inevitably result in having greater visibility and influence in society.
But Dr Fehoko says a modern western lifestyle in New Zealand has swept in a new reality.
“It used to be that our people had 10 or even 11, 12 children but now we’re seeing Pasifika families with only one or two kids.”
Dr Clark said by far the biggest factor affecting fertility was aging. Where Pacific people once started having families before embarking on careers, this was no longer the case.
“The biggest issue is female aging and what’s really interesting is that it’s not as old as you think.”
Meaning women in their mid 30s were now showing up at fertility clinics after struggling to conceive.
“As we push back having children [later], it’s going to become more and more of an issue.”
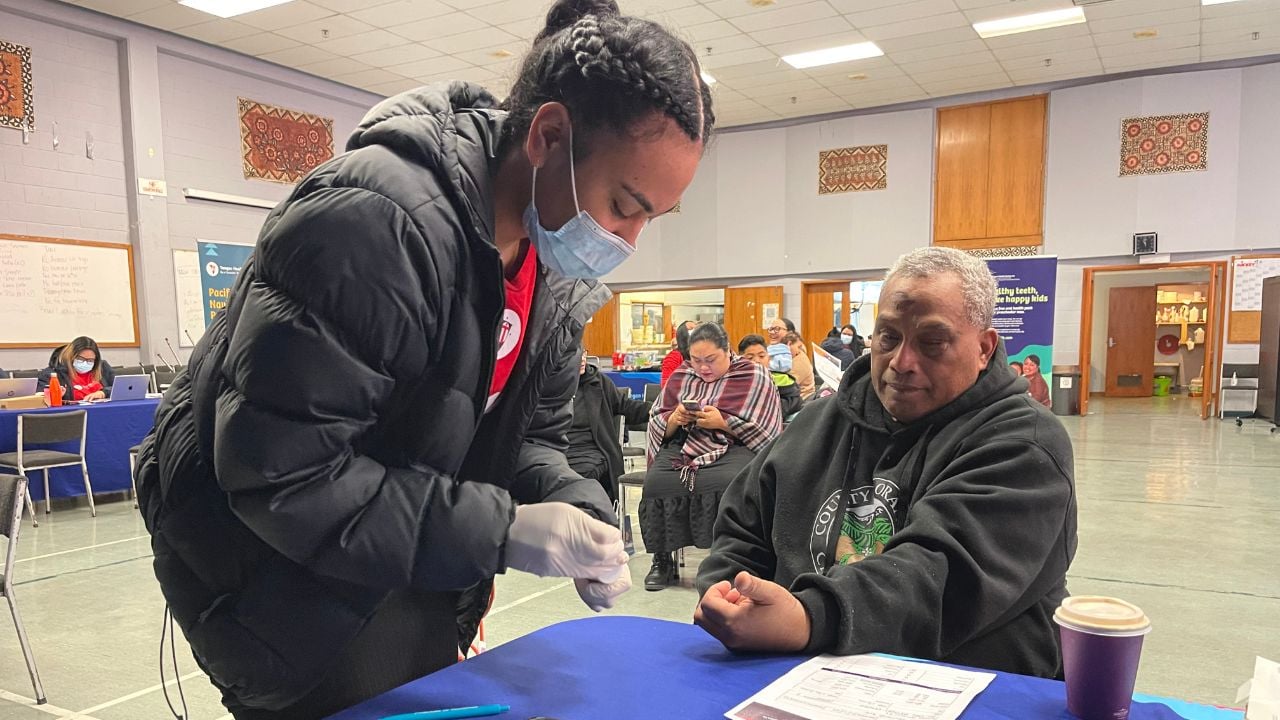
Dr Clark, a scientist, will undertake the first stage, collecting data to assess the numbers presenting at fertility clinics by ethnicity.
Both she and Dr Fehoko said for Pacific couples experiencing difficulties, the process itself was made even more problematic with the controversial use of Body Mass Index (BMI) as a criteria for publicly funded treatment to use assisted reproductive technology.
“It’s very demoralizing to walk into a room and even before you can get started, to be told you’re too fat,” said Dr Fehoko.
Dr Clark wants the research to challenge the criteria, labeling the justification as “loose” and that the study will collect BMI data in New Zealand to assess whether it correlates to the outcome and treatment.
“Sometimes it’s negative, sometimes there’s no impact, the justification is so loose… people come in and are higher than the [BMI] number, referring to Pacific patients who were told to come back after they had lost weight.
“The longer you wait, that’s time that people who come into the clinic don’t have,”
The subject of infertility isn’t a topic freely discussed in Pacific communities.
“We don’t talk about it enough, there are a lot of reasons we don’t understand,” Dr Fehoko said, pointing to what they hoped the second stage of talanoa within Pacific communities would reveal.
He emphasized the importance of having a family in Pacific cultures, to pass on land and titles, that this created even more pressure; as well as the debate around science versus faith compounding matters.
“At the end of the day if science is man-made, god made man, anything under that is a blessing. I’ll be looking at stories, attitudes, not just infertility but also seeing what their experiences have been through the clinics, drawing out key themes with data, to policies, to church groups.”
Samoan general practitioner Dr Aniva Lawrence and Academic Co-ordinator at the University of Auckland (Northland Clinical site) said low health literacy was another major factor. It required regular and on-going access to primary health care.
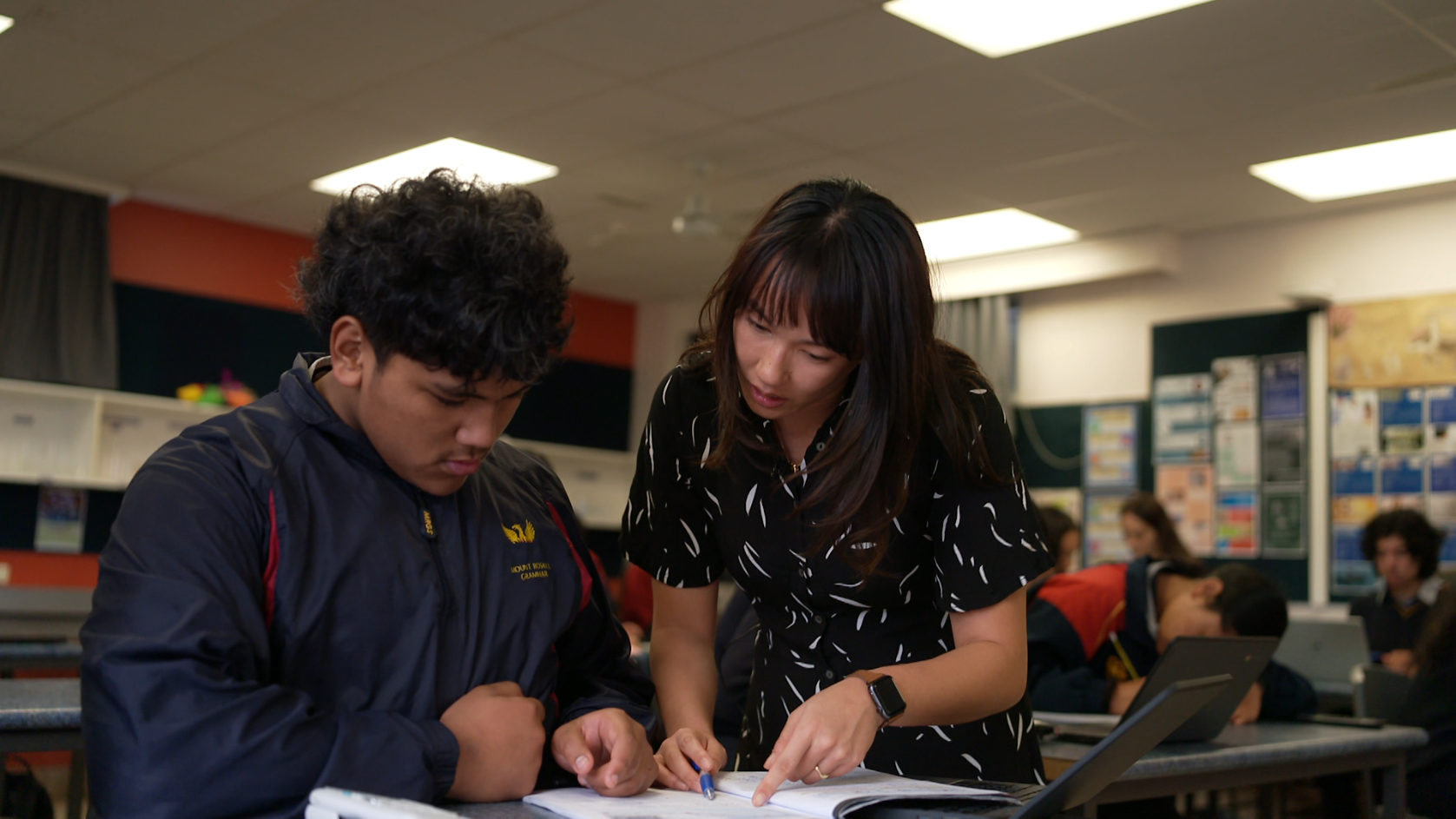
However low-income areas such as South Auckland tended to have fewer GP practices, with currently just two percent of practitioners from Pasifika backgrounds. Dr Lawrence said universities were undertaking a huge effort to train more Māori and Pasifika doctors requiring six years of study.
“These are personal issues, you’re not going to bring this up on the first consultation to a practitioner you don’t know,” highlighting the value of the GP-patient relationship.
She said colleagues were seeing higher rates of Polycystic ovary syndrome, Endometriosis as well as women of younger ages presenting with Endometrial cancer from Pacific communities.
“Unfortunately not experiencing periods is seen by some as a positive thing, you’re not having to pay for products and the inconvenience. But having a period is a positive thing,” she said, indicating good health in relation to fertility.
Secondary fertility issues were another phenomena, she said, explaining couples were sometimes able to produce one child but failed to get pregnant afterwards for a range of factors. These included trauma, stress that might stem from visa and residency issues, as well as poverty impacting on women’s health. Weight gain too would result in the issuing of a green prescription.
But Dr Lawrence said without access or resources to visit a nutritionist or dietician the issues persisted.
Sara (not her real name) said she suffered several miscarriages before having a second child with her first child now a teenager.
“My grandmother had her last child in her early 40s so I didn’t think it would be such a big deal getting pregnant at 35, but it was. The hardest thing was discovering nobody in my family or even our friends really wanted to talk about these things.”
Dr Fehoko and Dr Clark’s three year study will culminate in a symposium and they’re hoping to have Master’s students and PhD candidates support the research.