Public Interest Journalism funded through NZ On Air

By Kim Meredith of Local Democracy Reporting
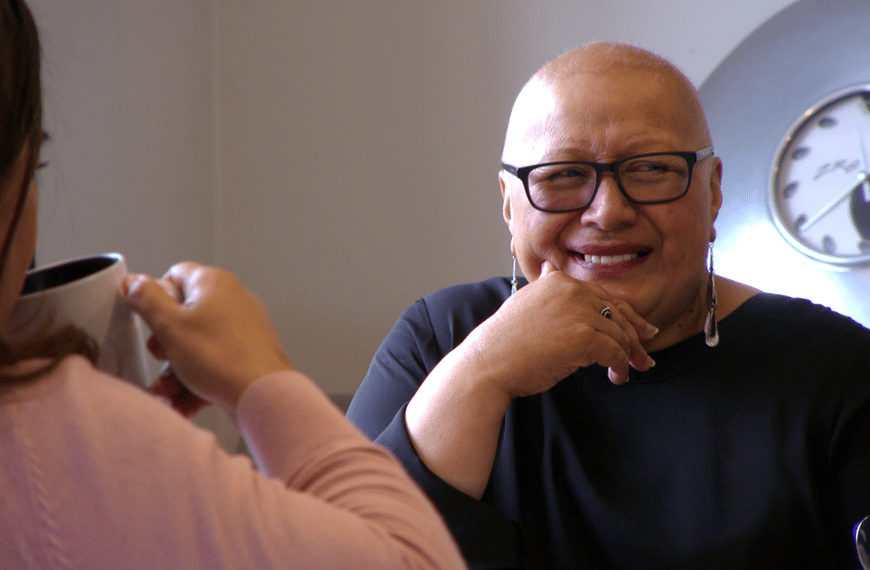
To address overwhelmed emergency departments (ED), more research is needed into why some Pacific patients are being steered towards hospitals like Middlemore, says a public health researcher.
Catherine J Yang, Public Health Registrar at the University of Auckland at the time of a 2019 study, says contrary to popular belief, Pacific participants do visit a health professional prior to visiting a hospital ED. And a repeat study, published last week, has thrown up more questions about the reasons people come into ED.
Previous studies by Counties Manukau Health have shown that Pacific patients are the highest ED users, and Yang says coming into winter, many EDs were overwhelmed, especially Middlemore Hospital.
For Malo Toe, he ended up at Middlemore as he was unable to make an appointment with his regular doctor, during a recent bout with cellulitis.
“I wasn’t sure where else could I go,” he says. “I mean what else are you going to do?”
Middlemore hospital has produced digital resources to educate the public around using alternative care before coming to its ED. But she believes more research is needed to determine why health professionals were steering some Pacific patients to EDs already under pressure.
With Pacific communities having settled in Aotearoa New Zealand more than 50 years ago, she says they were adept at navigating the health system; with many aware about seeking alternative health care providers.
However, she accepts Pacific cultural norms means any advice from health professionals would be followed to the letter, only for some to turn up at EDs and be told they don’t need to be at hospital.
“I know that for Asian families, it’s similar to Pacific families and what the doctor says, goes. You can feel shame.”
This can mean when people are turned away, there are ongoing consequences in being told that a condition didn’t warrant urgent attention.
“It could be a real missed opportunity, if someone feels shame and goes away not wanting to seek health care [later].”
Yang says it’s worth studying the reasons why GPs are referring patients to EDs and what other alternatives can be undertaken, as opposed to putting the onus solely on patients.
“More research is needed. Could resources be spent on better bolstering primary care?”
Mother of one, Joan Radford says she was proud of her late father who despite being a frequent visitor to the emergency department made the effort to shop around for his GP.
“My father was sick for a long time, he spent a lot of time in hospital but we were lucky to enjoy him for as long as we could. That came down to having good care from his GP. Most men avoid the doctor but my Samoan father was different, he visited the doctor at least once or twice a month.”
She says the same couldn’t be said for many of her fanau who didn’t have a regular GP, while she herself has been with the same GP for much of her adult life.
“Visiting the doctor isn’t cheap and for some of our people unfortunately it comes down to making a choice.”
Radford says with her father having been chronically ill for over a decade, she came to realise the importance of being a strong advocate for him.
“After you have visited the emergency department so many times, sat in the waiting room for countless hours and hours, you realise their focus is on making sure that whatever it is, [it] won’t kill you right there and then. It’s your GP who will treat you. But you have to be involved in whatever that looks like. That’s what we did with dad and we’re so grateful for the care he received.”