Health NZ says Middlemore Hospital’s under-pressure emergency department is continuing to adapt after a patient’s death last month and a surge in patient numbers due to winter illnesses.
But frontline staff say it’s business as usual, with patients still waiting up to eight hours to see a doctor.
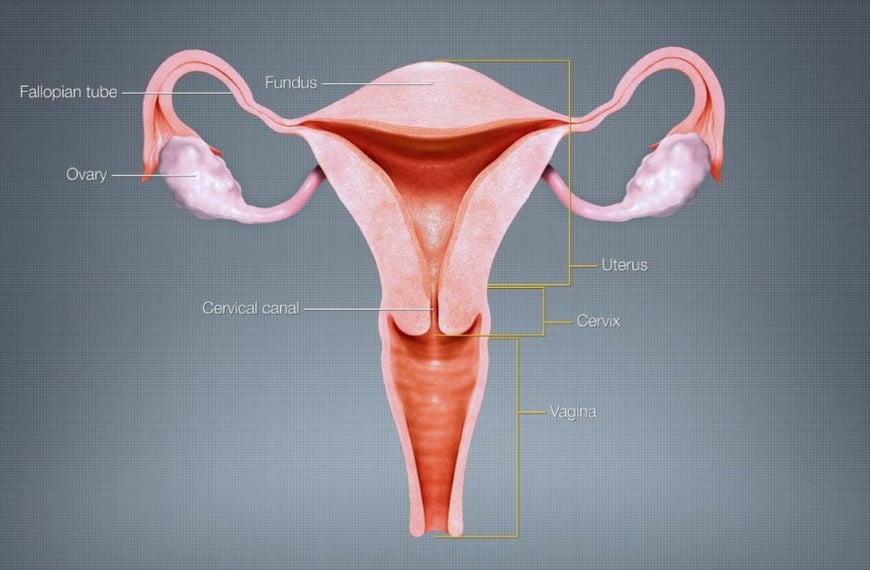
A patient died on June 16 after a “massive” brain haemorrhage. She had first arrived at Middlemore Hospital’s emergency department on June 15 with a severe headache.
She was told it would likely be hours before she could be seen, and left. The woman then returned to the hospital after suffering a brain haemorrhage and died the following day.
A doctor said she should have been given priority, despite the fact the emergency department was experiencing record admissions and long wait times for patients.
Te Whatu Ora (Health NZ) interim district director for Counties Manukau, Dr Pete Watson, said Middlemore Hospital was still under pressure due to a surge in respiratory illnesses, but it had taken steps to implement a winter response plan.
“This includes redeploying staff where possible to help mitigate pressure on our services, deferring non time critical surgery when necessary, and the recent temporary services of free weekend consultations and free pain relief for children in Counties Manukau district.”
He refused to answer questions regarding what changes had been made to the triaging of patients in its emergency department since the patient’s death.
Watson also didn’t respond to questions on when the final report as part of an investigation into the incident was expected, but did say once the review was complete it would provide a public statement.
But a senior healthcare worker from Middlemore Hospital’s ED, who didn’t want to be named, said there hadn’t been any noticeable changes to how patients were being assessed after the woman’s death last month.
And she said patients were still commonly waiting six to eight hours to see a doctor.
“We are aware of what happened, but there haven’t been any changes to how we are triaging patients,” she said.
“If you are really unwell you will be seen immediately, but if you aren’t there is a long wait time.”
And she said the hospital’s chronic staffing shortages, the increase in winter illnesses and Covid-19 and the fact people in south Auckland were waiting longer to see a GP, were only compounding the problem.
The Counties Manukau DHB ceased to exist on Friday under the Government’s health reforms and has been replaced by Te Whatu Ora (Health NZ).
Former chairman Mark Gosche was approached for comment at his Mt Wellington home on Monday about the patient’s death.
When asked if the board needed to take responsibility for the woman’s death, which happened during his tenure, he said it would be something that would be looked at in the inquiry.
“I don’t have the authority to speak now because I’m not the chair. We don’t exist as a board anymore and all of our responsibilities have shifted to Health NZ,” Gosche said.
“But they are carrying out a thorough investigation.”